What Happens If You Fail a Stress Test?
A stress test is an important tool used by a cardiologist to assess how your heart functions under physical activity. But that being said, what happens if you fail a stress test? Failing such a test can be pretty scary, but understanding the process and what comes next can help ease concerns and prepare you for the right steps forward.
At Apex Cardiology, we provide thorough and compassionate care through advanced stress testing designed to uncover any hidden heart issues and guide effective treatment. Let’s dive right in and discuss what comes after your stress test.
Understanding What a Stress Test Measures
While knowing why you failed a stress test matters, it can also be helpful to know what it was measuring in the first place. Stress testing evaluates how well your heart works when it’s pushed to beat faster and harder. This helps reveal problems that might not show up when your body is at rest.
What the test checks for:
- Blood flow to the heart muscle during exertion
- Heart rate and rhythm under stress
- Exercise capacity and endurance
- Symptoms like chest pain, shortness of breath, or dizziness during activity
By comparing your heart’s response during exercise to your resting state, your cardiologist gains valuable insights into potential heart disease or other cardiac concerns.
What Happens If You Fail a Stress Test?
When a stress test shows abnormal results, or in everyday terms, when you “fail” a stress test, it means your heart may not be getting enough blood flow during exertion. This can be a sign of coronary artery disease, irregular heart rhythms, or other cardiovascular problems.
Failing a stress test doesn’t automatically mean you have a severe heart condition. Instead, it signals the need for further evaluation. Your cardiologist will carefully review your results along with your symptoms, medical history, and risk factors to determine the best next steps.
Common Follow-Up Actions After a Failed Stress Test
If your stress test indicates potential issues, your cardiologist may recommend one or more of the following:
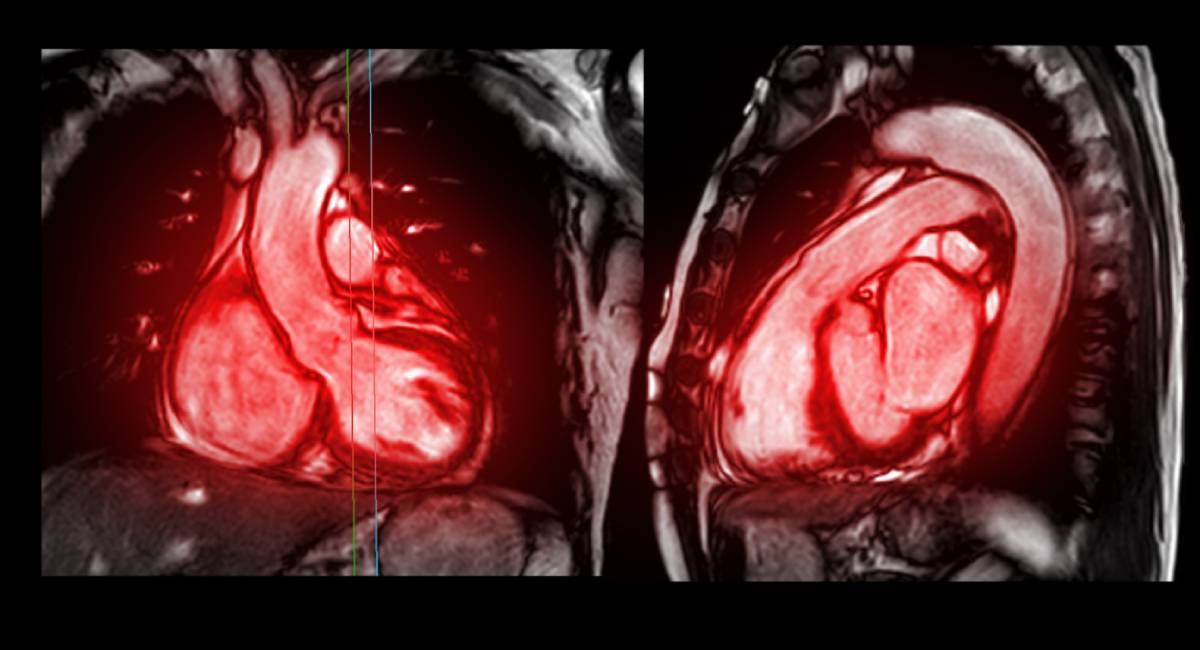
- Additional diagnostic tests, such as echocardiograms, nuclear imaging, or coronary angiography, may be performed to get a clearer picture of your heart’s health.
- Lifestyle modifications like diet changes, quitting smoking, or increasing physical activity tailored to your condition.
- Medications to manage symptoms or reduce risks, such as blood thinners, cholesterol-lowering drugs, or beta blockers.
- Procedures or interventions, including angioplasty or stent placement if blockages are detected.
- Each patient’s plan is unique, designed to address their specific needs and improve heart function safely.
What To Expect After Failing a Stress Test
- Learning you failed a stress test can be unsettling. However, it’s important to remember that the test is only one piece of the puzzle. Your cardiologist at Apex Cardiology will work closely with you to:
- Explain your test results in clear, understandable terms
- Answer your questions and discuss any symptoms you may be experiencing
- Develop a step-by-step care plan based on the findings
- Schedule further tests or follow-ups as needed
This personalized approach helps make sure that you get the care you need with as little worry as possible.
How Stress Testing Supports Long-Term Heart Health
Even if you pass your stress test with flying colors, this test is a valuable tool for monitoring your heart health over time. For those who fail, it provides critical information that can prevent serious complications through early detection and intervention.
Regular check-ins and follow-up stress tests may be recommended based on your risk factors and heart condition.
Taking the Next Step Toward Heart Wellness
Failing a stress test is not the end of the road—it’s an opportunity to take charge of your heart health with the guidance of skilled professionals. At Apex Cardiology, our team of expert cardiologists is ready to support you through every step of diagnosis and treatment. Contact us today to schedule a consultation and get the answers and care you deserve.